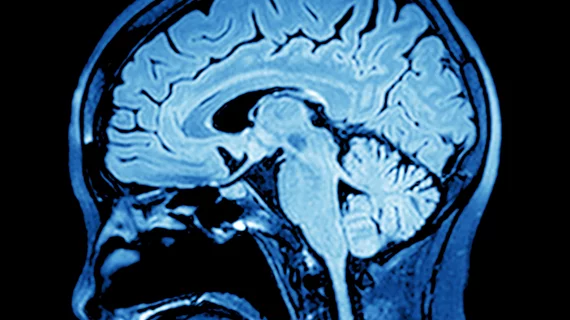
An advanced mapping technique detected trace amounts of gadolinium in the brain that were not measurable using conventional MRI scanning, according to a new study published Tuesday.
Radiologists from South Korea analyzed nearly 100 patients with brain tumors, spotting tissue changes associated with repeated macrocyclic gadolinium-based contrast agent injections on quantitative susceptibility mapping (QSM), but not standard T1-weighted MRI.
These findings, available in Radiology, should serve as a “wake-up call” to the limitations of the latter approach in detecting gadolinium retention, and an “opportunity” for improved detection via QSM, Weill Cornell Medicine radiologists wrote in an accompanying editorial.
“This spectacular improvement in the ability to noninvasively detect trace amounts of gadolinium in the brain by using QSM verifies that macrocyclic GBCA accumulates in the brain,” Yi Wang, PhD, and Martin R. Prince, MD, PhD, both with the New York university, added.
The pair also believes that the imaging information gathered during routine MRIs—known as gradient-echo data—can be used to reduce required GBCA dosage, illuminate deposition pathways and clarify clinical ramifications. It will require performing QSM during such exams, which can be a big computational hurdle, but ideally would be automated into the postprocessing protocol for commercial scanners.
For their July 21 study, the researchers retrospectively analyzed 199 MRI scans from 90 patients performed between August 2014 and February 2019. Gadobutrol was the only GBCA used for follow-up MRI, with a mean of eight injections.
First author Yangsean Choi, and colleagues at Seoul Saint Mary’s Hospital’s College of Medicine, discovered that the magnetic susceptibility of the globus pallidus—a structure in the brain involved in regulating voluntary movement—increased by 1.4 parts per billion for each gadobutrol administration. This remained the case after adjusting for cofounders, and there was no association between the number of injections and magnetic susceptibility in the dentate nucleus.
“Our findings demonstrated that there might be [a] positive association between magnetic susceptibility of the GP and repeated exposure to gadobutrol,” the authors wrote.
GBCA administration and deposition remain hotly-contested issues, especially as they relate to mitigating radiologists’ liability exposure to suits claiming gadolinium deposition disease. And experts recently went back and forth over the best approach in pieces published by JACR.
“In summary, Choi et al demonstrated that QSM is highly sensitive in the detection of small quantities of gadolinium deposition in the brain after macrocyclic GBCA administration,” the Weill Cornell editorialists concluded. “This is a wake-up call regarding the limitations of routine T1-weighted imaging in detecting gadolinium enhancement and/or retention and the opportunity for much higher sensitivity by using QSM.”
Choi and colleagues disclosed no relevant conflicts of interest in their research. The Cornell Medicine clinicians disclosed patents for QSM owned by the university and stock options in Medimagemetric.
Related MRI Contrast Agent Safety Content:
A deep dive into gadolinium-based adverse reactions
Allergic reactions to iodinated CT contrast increase likelihood of sensitivity to GBCAs
Researchers detail data on gadolinium-related adverse reactions
Radiologists must take a data-driven approach to discuss gadolinium, mitigate liability risk
Radiologists see potential to reduce GBCA administration with new synthetic MRI technique
Gadolinium-based contrast agents are safe, even at higher doses, new research suggests
Gadolinium debate rages on, with radiologist questioning recent GBCA liability guidance
ACR committee proposes new term for symptoms associated with gadolinium exposure
Closing the knowledge gap on gadolinium retention risks
Radiologists find direct evidence linking gadolinium-based contrast agent to higher retention rates
AI software that eliminates need for gadolinium contrast during imaging exams wins patent
Research may offer new method to detect GBCA on MRI
Radiology, other multispecialty groups urge caution with GBCAs during interventional pain procedures
Cardiac MRI contrast agents are low-risk and safe for ‘overwhelming’ majority of patients
Health orgs publish special report about gadolinium retention, GBCA use in imaging
Rodent brains retain gadolinium after repeated administration of GBCA a year after injection
Radiologists should keep patients’ best interests in mind to mitigate gadolinium liability risk