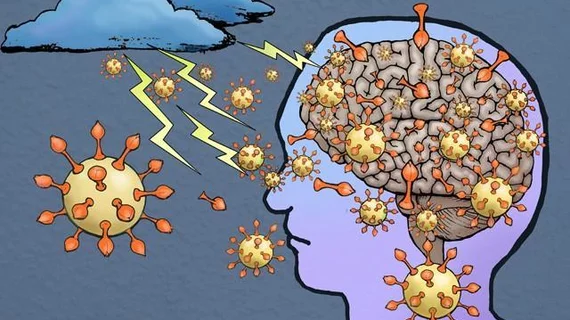
New research published this week suggests COVID-19 can cross the blood-brain barrier. The finding gives credence to the many patients who complain of lingering cognitive side effects long after contracting the disease.
University of Washington School of Medicine researchers in Seattle led the study, which looked at how the coronavirus spike protein behaves in mice. This S1 protein, they found, can cross the blood-brain barrier and grab onto other cell receptors which may be toxic to brain tissue.
When the immune system sees the virus and its proteins, it tries to kill the invader and leaves an individual with brain fog, fatigue and other cognitive issues, lead author William A. Banks, MD, a professor at UW Medicine, wrote Dec. 16 in Nature Neuroscience.
"We know that when you have the COVID-19 infection you have trouble breathing and that's because there's infection in your lung, but an additional explanation is that the virus enters the respiratory centers of the brain and causes problems there as well," Banks explained in a statement published Friday.
Imaging has played a key role in uncovering the brain abnormalities in patients with adverse neurological symptoms. A study published earlier this year spotted three distinct neurological patterns on imaging, with signal abnormalities in the medial temporal lobe accounting for 43% of cases. Extensive and isolated white matter microhemorrhaging was noted in nearly a quarter of the group.
Another investigation published in July found that those admitted to the emergency department with neurological symptoms are 2.4 times more likely to suffer large vessel occlusion stroke compared to healthy patients. There’s still much unknown, however, about how the virus attacks the central nervous system.
Looking over the results of this study, Banks found the S1 protein in COVID-19 behaves almost exactly the same as the gp 120 protein in HIV-1. Banks and colleagues study the blood-brain barrier in Alzheimer’s disease, obesity, diabetes, and HIV, but in April dropped all their efforts to focus on the S1 protein and the coronavirus.
"You do not want to mess with this virus," he added. "Many of the effects that the COVID virus has could be accentuated or perpetuated or even caused by virus getting in the brain and those effects could last for a very long time."