When patients with substance dependence issues are shown cues or images related to such substances, activity in a specific area of the brain increases, according to an fMRI-based study published in Translational Psychiatry. The results may have implications for addiction treatment.
Colleen A. Hanlon, PhD, of the Medical University of South Carolina (MUSC) and colleagues recruited 156 patients—55 chronic cocaine users, 53 heavy alcohol users and 48 current cigarettes smokers—for their study. Patients were shown images of these substances which were alternated with corresponding neutral images. During the task, researchers imaged brain activity using fMRI.
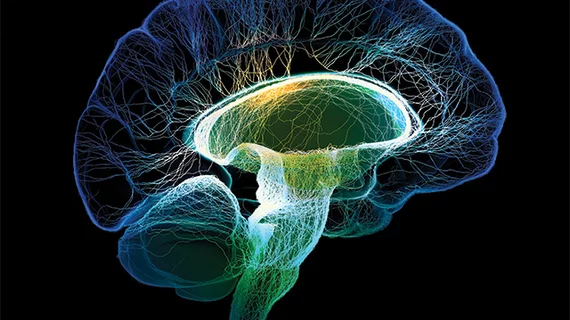
When presented with drug and alcohol cues, all three groups of participants demonstrated “hot spots” in the medial prefrontal cortex (mPFC)—an area of the brain which includes memory retrieval and the limbic reward circuit, according to the researchers.
"As we move forward into clinical trials, these findings suggest that, by modulating the mPFC, we might be able to help multiple forms of substance-dependent populations, rather than having to reinvent the wheel for every particular disease," Hanlon said in a MUSC news story.
Phase 2 clinical trials are currently underway for patients seeking treatment for cocaine or alcohol use. Those groups receive fMRIs during the first week of the study and are subsequently randomized and offered 10 days of transcranial magnetic stimulation (TMS) therapy or a placebo therapy. Scans are performed after inpatient treatment and at one and two month post-treatment to determine if cue-reactivity is reduced .
TMS therapy balances neural networks in the brain by emitting a magnetic field to certain areas to either constrict or stimulate electrical activity. It has few side effects, and is used as a treatment option for depression.
"It's a really exciting time to be in the field," Hanlon said in the same story. "We have decades of preclinical research that have demonstrated specific neural circuits involved in drug use, and we have lots of clinical research that has developed various pharmacological agents, but we don't have any neural circuit-based interventions