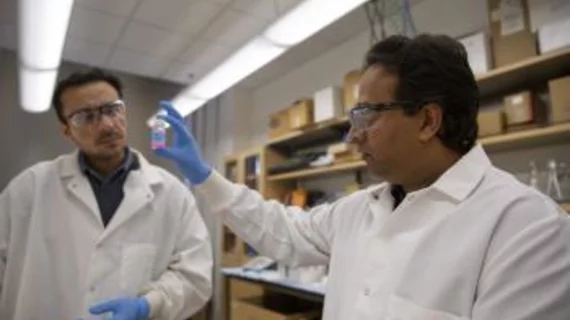
Vikram Kodibagkar, PhD, an associate professor of engineering at Arizona State University (ASU) in Tempe, has been researching a new way to measure tissue oxygenation using advanced 3D imaging for the past four years.
His goal? To find a noninvasive technique that measures the amount of oxygen present in tissue—called tissue oxygenation—which could ultimately help create more effective treatments for cancer and other conditions, according to a recent ASU news release.
“Knowing about the oxygenation (of tissues) might allow us to tailor the therapy to make it better and to use other therapeutic interventions that are more appropriate,” said Kodibagkar, whose research was funded by a 2014 National Science Foundation CAREER award.
Kodibagkar also leads the Prognostic Bioengineering Lab at ASU, which has a mission to develop new imaging technologies that detect changes in tissue microenvironments and to train new leaders in biomedical imaging.
The technique
When a cancerous tumor grows, it outgrows its blood supply and leaves parts of the tumor deprived of oxygen, or in a hypoxic state. Standard therapies to treat tumors such as radiotherapy are not typically effective in hypoxic regions, however Kodibagkar’s new technique may be.
Using his tissue-oxygenation measuring technique to provide information about the locations of hypoxic areas, radiologists could increase the dosage of radiotherapy where tumors pose the greatest risk of metastasizing. The application could also be used for therapies beyond cancer, such as for patients with traumatic brain injury (TBI) or those who have suffered a stroke or heart attack, according to the release.
The success of the technique is based on the perfusion of the imaging contrast agent and its retention in hypoxic areas, according to the release.
While the contrast agent is outside of both the blood vessels and cells, Kodibagkar’s team used MRI scanners to document how much the contrast agent binds to its surroundings. If a contrast agent accumulates in a region of tissue, the researchers assume it has passed through damaged blood vessels, which are commonly found in tumors or may be a result of TBI.
If the team’s newly developed contrast agent is retained three hours or more, the researchers assume the presence of hypoxia in the tissue.
Kodibagkar and his team also uses pharmacokinetic modeling (a mathematical technique used to predict the absorption, distribution metabolism and excretion of synthetic or natural chemical substances in the body) to detail the contrast agent’s movement, using 3D imaging to create calibration phantoms that can simulate different conditions in the body. The phantoms are then scanned with MRI to evaluate the performance of an imaging agent and correlate its results with controlled environmental changes.
The data collected are fit to a pharmacokinetic model to extract quantitative information about oxygenation based on the imaging data, according to the release.
The team also had to redesign the calibration phantom and synthesize their own contrast agent to due costs as buying a custom-made contrast agent would be too expensive, which Kodibagkar said worked out for the better.
“One unexpected takeaway message for the world is that we’ve developed an agent that does both perfusion and hypoxia imaging,” Kodibagkar said. “In that sense, it would be superior to a commercial contrast agent.”