New research offers radiologists guidance in differentiating between COVID vaccine-related swelling of the glands from malignant adenopathy based on specific features identified using ultrasound.
Unilateral axillary adenopathy is a known side effect of COVID vaccines. The increased instances of axillary lymphadenopathy post-vaccine initially caused experts to advise women to delay their annual mammographic screenings, as many of them were having to undergo additional imaging and procedures to confirm that their swollen lymph nodes were benign. Research has since suggested that the adenopathy can sometimes persist for many months and that mammograms should not be delayed due to the COVID vaccine.
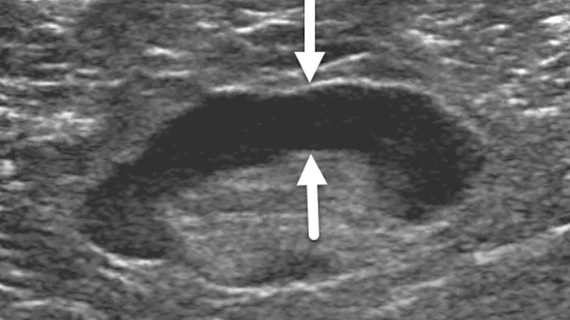
Individuals who have abnormal lymph nodes identified on imaging are frequently sent for ultrasound. The modality is a valuable diagnostic tool when it comes to characterizing adenopathy, but experts note that there is some overlap between the appearance of benign and malignant nodes, which can make diagnosing their root causes challenging.
With the number of individuals who are eligible to receive COVID vaccines and boosters continuing to rise, it is important to understand how lymph nodes with benign versus cancerous origins present on imaging.
“Objectively differentiating benign from malignant adenopathy is of clinical value and can reduce costs and anxiety related to unnecessary biopsies and/or the need for follow-up examinations,” corresponding study author Chung HL, from the department of breast imaging at the University of Texas MD Anderson Cancer Center, and co-authors wrote.
To better comprehend this concern, researchers compared the lymph node features in benign, vaccine-related adenopathy to those of biopsy-proven malignant adenopathy witnessed in breast cancer patients.
The results of their work revealed cortical thickness and its morphology to be the most reliable features in distinguishing benign nodes from malignant ones. The average cortical thickness for the benign nodes was 5.1 mm, compared to 8.9 mm for the malignant nodes. Their research indicated that increasing the threshold cortical thickness cutoff to ≥ 5.4 mm yielded more accurate malignancy diagnoses than the current 3 mm cutoff.
The presence of three or fewer swollen nodes also increased the likelihood of malignancy, and all of the nodes that were completely hypoechoic and without visible hila were found to be cancerous as well.
“These considerations will be important as more patients receive COVID-19 vaccines for the first time or receive additional booster vaccines,” the authors suggested.
You can view the detailed research and find more images in the Academic Radiology article.
Related COVID vaccine-induced adenopathy in breast imaging:
Mammograms should not be delayed after COVID vaccine, research shows
Q&A: Should COVID vaccinated patients delay getting breast imaging — new study says no
How radiology providers can minimize mammography recalls among COVID-vaccinated patients
Most routine imaging should be scheduled 6 weeks after 2nd vaccine dose, major cancer centers say
Managing COVID-19 vaccine side effects: Harvard radiologists share their ‘pragmatic’ approach
COVID-19 vaccine update: Radiologists report side effects mimicking breast cancer on mammograms