There are not yet consensus-based guidelines available for screening women with dense breast tissue, so researchers at Mayo Clinic recently developed a set of recommendations regarding supplemental breast imaging.
Study author Suneela Vegunta, MD, a women's health specialist at Mayo Clinic in Arizona, said randomized controlled studies that review the effect of supplemental screening versus mammography alone for breast cancer mortality have not yet been performed. She says these studies, along with guidelines for screening women with dense breast tissue, are needed.
"One challenge for some women is dense breast tissue," Vegunta said in a statement about the study. "Dense breast tissue is an independent risk factor for breast cancer and may also mask small breast cancers, thereby reducing the sensitivity of a screening mammogram. Dense breast tissue is an independent risk factor for breast cancer and may also mask small breast cancers, thereby reducing the sensitivity of a screening mammogram."
She explained there are millions of women in the U.S. with dense breast tissue and it is found in nearly half of women eligible for breast cancer screening, particularly in younger women. She also noted that breast density may decrease after menopause.
Legislation requiring providers to notify women about their breast density was passed in several states, which has made more women aware of their breast density. Dense tissue often requires supplemental imaging to see through the tissue to look for cancers, including use of breast ultrasound, MRI, and nuclear imaging. The issue of dense breasts has also led to wider adoption of tomosynthesis 3D mammography systems, and nearly all breast imaging centers have at least on of these systems today.
"Supplemental breast cancer screening modalities can help diagnose additional cancers that are possibly masked by dense breast tissue on mammograms," Vegunta explained. "Our paper provides information and guidance for healthcare professionals and patients on the benefits and drawbacks of various supplemental screening modalities in the background of using a risk-based stratification of patients with dense breast tissue."
Expanding use of Digital Breast Tomosynthesis
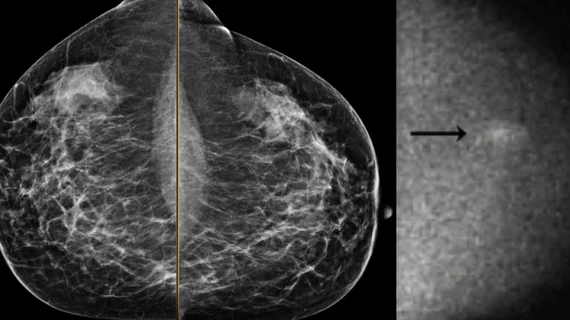
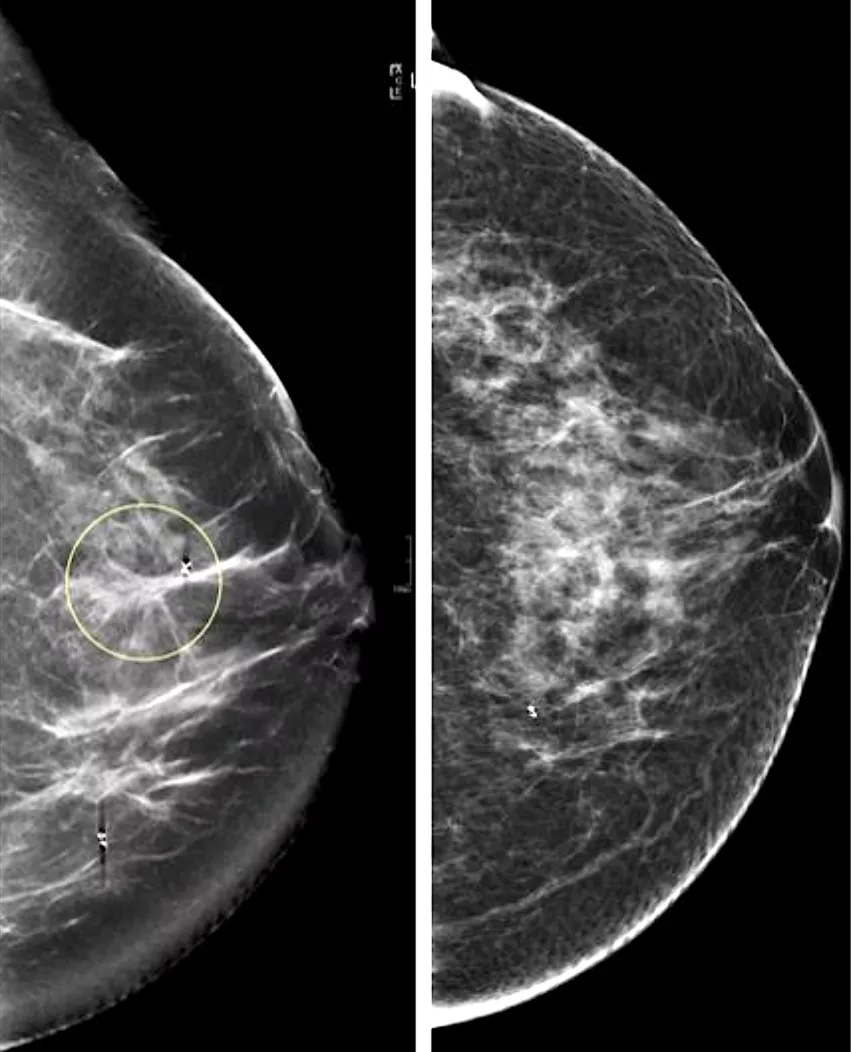
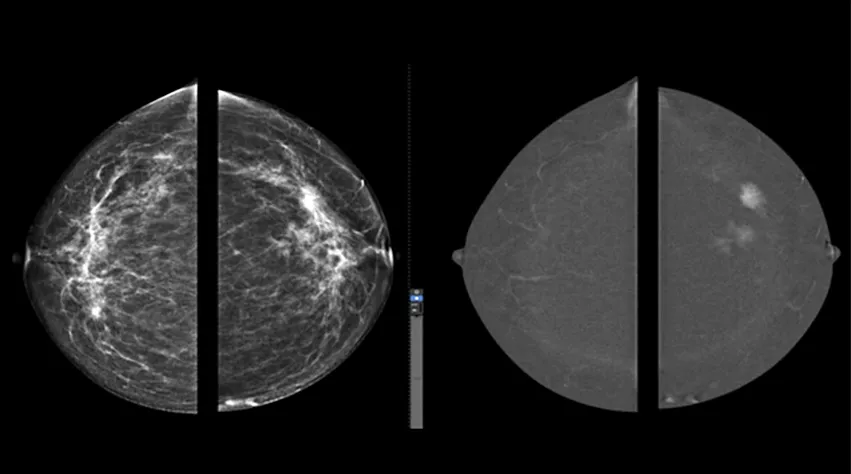
Digital breast tomosynthesis (DBT), also known as 3D mammography, collects a series of images as the X-ray head moves in an arc over the breast from multiple angles. This allows image reconstruction of the breast as a dataset where the radiologist can flip through a series of images, usually with a 1 mm slice thickness. Vegunta said the thin images reduce the overlap of tissues and help with the separation of breast lesions from superimposed breast tissue to improve lesion conspicuity.
Studies have shown an additional 1.2 to 2.7 cancers detected per 1,000 screening examinations using 3D mammography compared with standard 2D digital mammography. The study researchers said the increased sensitivity enables a reduction in recall rates of 0.8% to 3.6%, and a reduction in false-positive recall rates of 29%.
"At Mayo Clinic, this is standard. We offer 3D mammography to all of our patients," Vegunta said in a video included as supplemental material with the paper. "The reason for this is because tomosynthesis produces less breast pain so patients tolerate these mammograms better. It also reduces the recall rates."
She added the the modality also finds additional cancers missed on 2D mammography.
A comparison of standard 2D mammography (right) and digital breast tomosynthesis (DBT), or 3D mammography (left). The DBT creates a data set of 1 mm slices that the radiologist can look through to see more detail in suspect areas and determine if it dense breast tissue is masking a tumor. Image from UCSF.
Breast ultrasound is the most widely available supplemental imaging
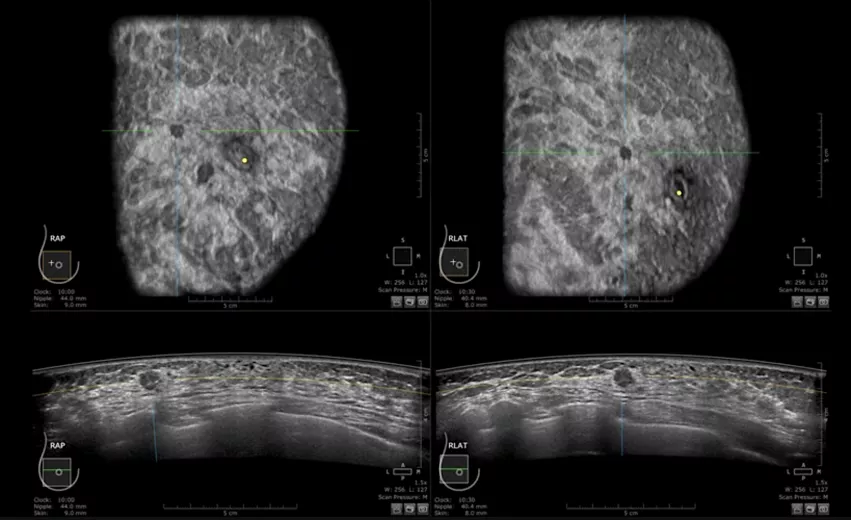
Breast ultrasonography is widely accessible in the United States and allows real-time imaging during lesion biopsies. Whole-breast ultrasonography (WBUS) has become a common supplemental screening.
Vegunta et al. states in their guidance that handheld sonography has the drawback of scan reproducibility and requires a highly trained breast imaging specialist. Ultrasound also lacks the spatial resolution of mammography and does not help in the diagnosis of most microcalcifications. But, it does differentiate tissues of varying densities, including fluid vs. soft tissue.
"Ultrasound can have a significantly high false positive rate, but the advantages are that is is widely available," Vegunta said.
The cancers missed on mammography but detected by ultrasound are reported to be mostly small, node-negative and invasive breast cancers, the authors report. About 1.8 to 4.6 additional breast cancers were detected per 1,000 women when WBUS was used for screening asymptomatic women with dense breasts and normal results on mammography. More than 70% of these cancers were less than 10 mm, 90% were stage 0 or 1, and 94% were invasive, the researchers found.
Interval cancer rates have been shown to be reduced after the introduction of ultrasound screening as a supplemental study, the authors wrote.
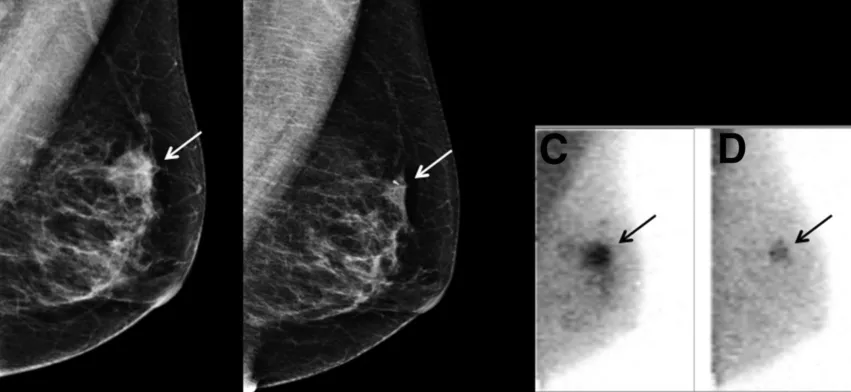
Molecular breast imaging can show metabolic changes in breast tissue due to cancer
Molecular breast imaging (MBI) is a functional nuclear imaging test that uses a tumor-avid radioactive tracer, technetium Tc 99m sestamibi, the paper states. The imaging can show vascular and metabolic changes in breast tissue, which may show growth of a tumor. Cancer cells have a higher cellular metabolism compared to health tissue. This faster metabolism results in greater uptake of the technetium radiotracer and shows up as a bright spot in the nuclear image. But the authors note nuclear imaging has limitations on anatomic details.
MBI detected an incremental 7.5 to 8.8 cancers per 1,000 women screened, and only a small decrease in specificity, the authors found.
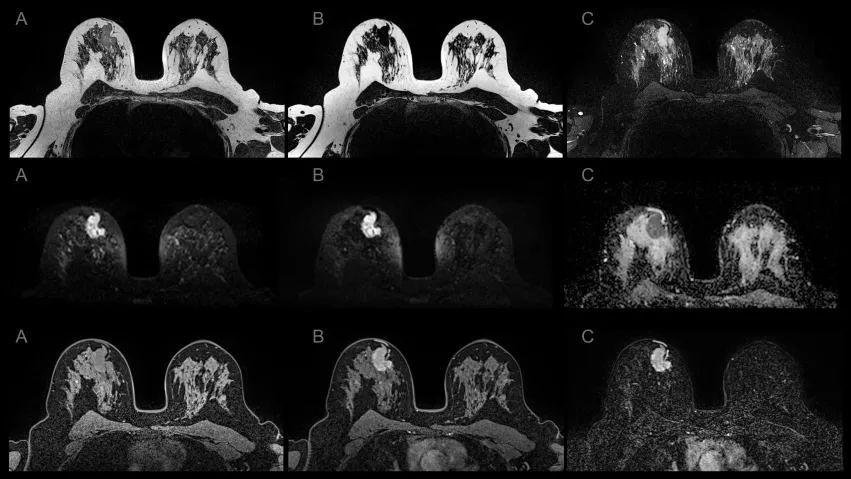
Breast magnetic resonance imaging has higher sensitivity in high-risk patients
The authors said MRI has higher sensitivity than mammography or ultrasonography alone for breast cancer detection in the high-risk population. The ACR recommends MRI in conjunction with mammography for screening of high-risk women who have a lifetime risk of breast cancer that exceeds 20% on the basis of the Tyrer-Cuzick risk assessment model, also called the International Breast Cancer Intervention Study (IBIS) Tool.
High-risk women include those who are who are carriers of the BRCA1 and BRCA2 gene variant, Li-Fraumeni syndrome or Cowden syndrome and those who received radiation therapy for Hodgkin lymphoma, according to the researchers. Several other genetic mutations mentioned in the paper are also associated with higher risk.
"Breast MRI is probably the most sensitive of all the breast screen modalities, so that means it picks up more cancers," Vegunta explained. "In a study it picked up more than 18 per 1,000 women screened, who actually presented with a negative mammogram."
She said a future direction of MRI is breast MRI abbreviated fast protocols, which only will take about 5 minutes to perform, greatly shortening exam times.
Contrast-enhanced mammography is an emerging diagnostic imaging tool
Contrast-enhanced mammography (CEM) is a newer imaging method that uses standard low-energy and recombined, subtracted mammography images obtained in standard views after injection of iodinated contrast. It provides high-resolution anatomic and physiologic contrast-enhanced information to evaluate tumor neovascularity, the authors wrote. CEM has shown superior diagnostic accuracy compared to traditional 2D mammography in studies. The researchers said CEM is not currently used as a supplemental screening tool in average-risk women with dense breasts, except under off-label or research purposes.
Read the full text in the November 2021 issue of Mayo Clinic Proceedings.[1]
Related breast imaging technology content:
DBT plus synthesized mammography drops patients’ dosage without losing imaging quality
3D mammography approaching 50% of breast imaging systems in the US
Ultrasound alone detects 92% of breast cancers recalled on DBT exams
Breast MRI screening cuts cancer mortality rates in half for women with lesser-known gene mutations
DBT spot compression views increase reader accuracy
Digital breast tomosynthesis outperforms DM at detecting malignancy in developing asymmetries
AI drops DBT workloads for radiologists by 40% while also reducing recalls
Less experienced radiologists are more susceptible to fatigue when reading DBT exams
Stand-alone AI can reduce radiologists’ screening mammography workloads by 90%
Imaging center has credentials revoked following ‘severe’ issues with mammography screening
Q&A: Should COVID vaccinated patients delay getting breast imaging — new study says no
Reference: