With the overtreatment of lung cancer becoming a growing concern in the medical community, researchers are looking for ways to narrow patient cohorts down to those who are at the greatest risk of poor outcomes due to the deadly disease.
One means of achieving this is through the growing field of radiomics, which can identify minute patterns and features in medical imaging that human readers may be unable to detect. A new study published in Cancer Biomarkers analyzed the effectiveness of using radiomics features to stratify risk and predict outcomes of patients whose lung cancer was spotted on low dose computed tomography (LDCT) screening. In the study, experts shared how they were able to develop a radiomics model that can accurately categorize patients’ level of risk for poor lung cancer outcomes and thus help to guide clinicians in choosing appropriate treatment strategies.
“Overtreatment is a serious adverse effect of cancer screening and early detection,” corresponding author Matthew B. Schabath, PhD, from the Department of Cancer Epidemiology at H. Lee Moffitt Cancer Center and Research Institute in Tampa, Florida, and co-authors explained. “Identifying patients that have aggressive, high-risk tumors associated with very poor survival outcomes would help oncologists decide which patients may need more aggressive treatment, such as adjuvant therapies. On the other hand, patients that have less aggressive, low-risk tumors have a better chance of cure by surgery and may not need adjuvant therapies.”
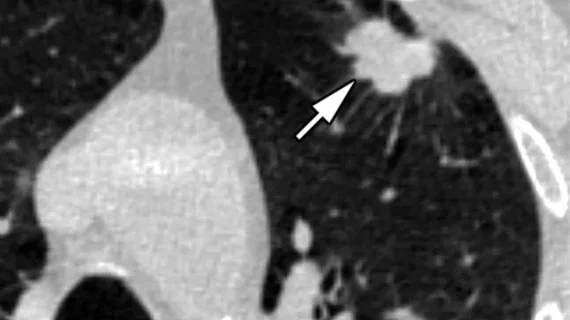
Researchers at Moffitt Cancer Center acquired images from the National Lung Cancer Screening Trial to extract tumor features that could be used to categorize risk. Patients whose imaging was included in the research had two scans approximately one year apart. Peritumoral and intratumoral radiomics were extracted from the initial screening. Volume doubling time (VDT) was calculated based on scans obtained at baseline and follow-up and was combined with the radiomic feature of compactness to develop the researchers’ predictive model.
The model divided patients into 3 groups—low, intermediate and high risk. A 5-year overall survival of 25% was recorded for the high-risk group, compared to 83.3% for the low-risk category. Poorer outcomes were also observed in the high-risk group for those who were diagnosed with lung cancer during its early stages, with a 5-year overall survival of 44.4% compared to 90.9% in the low-risk group. Researchers were also able to identify a VDT cut-point of 279 days that differentiated aggressive from low-risk cancers.
“The results from our analyses revealed that radiomics combined with volume doubling time can identify a vulnerable subset of screen-detected lung cancers that are associated with poor survival outcomes, suggesting that such patients may need more aggressive treatment. We hope to do further studies to validate our findings before applying our model to patient care,” said Jaileene Pérez-Morales, PhD, a postdoctoral fellow in the Cancer Epidemiology Department.
Related cancer screening content:
AI-based mammo screening protocol reduces radiologist workload by 62%
Experts highlight 'suboptimal' rates of CMS-required shared decision making encounters prior to LDCT
'Surprising' decline in annual screening among breast cancer survivors has experts concerned
Lung cancer screenings are proven to save lives, but disparities remain, experts discover