An estimated 40 million diagnostic imaging errors occur around the globe each year, increasing morbidity and mortality rates while wasting healthcare dollars.
Head and neck imaging is particularly susceptible to mistakes, Reza Assadsangabi, MD, with the Division of Neuroradiology at the University of California-Davis, and co-authors suggested Friday. But radiologists can take measures to educate themselves and avoid such misdiagnoses.
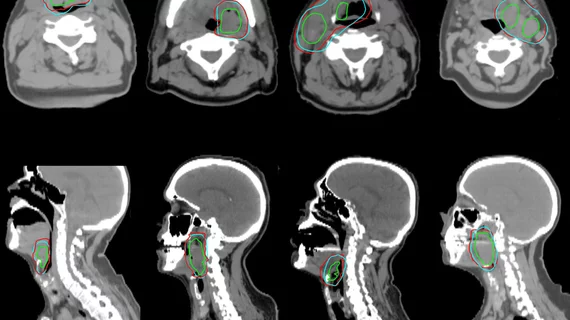
“Complex anatomy and a wide spectrum of diseases in the head and neck predispose interpretation of neck imaging to cognitive pitfalls and perceptual errors,” the authors added. “Extra attention to common blind spots in the neck and familiarity with common interpretive challenges could aid radiologists in preventing these diagnostic errors.”
The neuroradiologists pooled their experience and shared tips for overcoming these challenges in a new piece published Nov. 5 in Clinical Imaging.
1). Radiologists must develop an expert understanding of neck anatomy, including parts of the brain and upper thorax. Knowledge of common blind spots, such as thrombosis at the base of the skull in cancer patients, is also important, the authors noted.
2). Standardized terms should be used during reporting, while structured templates to describe abnormalities can encourage dialogue between radiologists and other clinicians.
3). Review images using a systematic approach and checklist of often-overlooked features, including soft tissue exams with possible vessel stenosis and thyroid lesions at the boundaries of imaging exams, among many other potential abnormalities.
4). Don’t hesitate to consult with more experienced radiologists or other colleagues when reading head and neck exams, and refer to available literature often.
5). Reach out to referring physicians when a patient’s history or physical findings are incomplete or indeterminate.
6). Oncology reporting checklists may benefit from utilizing aspects of TNM staging, which describes the size of the tumor, spread into nearby tissue and lymph nodes, and metastasis throughout the body.
Read the full study for more, including breakdowns by individual anatomic areas.